In true pathogenic fungus infections, the fungus is virulent regardless of the constitutional adequacy of the host. True pathogenic fungi include Histoplasma, Coccidioides, Blastomyces, and Paracoccidiodies.
- Pathogenicity is an accidental phenomenon and is not essential to the survival or dissemination of the species involved. Most infections are either completely asympotmatic or of very short duration and quickly resolved. Resolution of the infection is accompanied by a strong specific resistance to reinfection that is of long duration.
- very restricted geographic distribution of fungus
- sex, age, and race are important factors in the statistics of pathogenic fungus infections
- pathogenic fungi exhibit a morphological transition from a the mycelial or saprobic form to the parasitic form found in infected tissue. Thermal dimorphism is common!
- chronic granulomatous and suppurative (bleeding pus) disease having a primary pulmonary stage that is frequently followed by dissemination to other body sites (e.g., skin and bone).
- occurs in humans and dogs (also seen in horses, wild animals, northern sea lion).
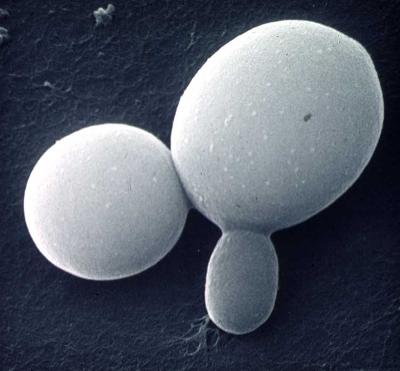
- anamorph, asexual, or imperfect form of fungus, Blastomyces dermatitidis is the etiological agent (perfect form of this fungus is Ajellomyces dermatitidis, an ascomycete).
- dimorphic or diphasic fungus (converts from filamentous form to yeast form and vice versa)
- soil saprophyte (erratic distribution, grows on decaying organic materials).
- some evidence for presence of disease in Middle Eastern countries, Africa, India, South America.
- Discovered in 1890's by Caspar Gilchrist
- diseases acquired through inhalation of conidia
- primary cutaneous disease is rare.
- very rare are reported cases of infection by yeast phase through (a) sexual transmission (from man to woman), (b) person-to-person, or (c) animal to person contact.
- chronic pulmonary and disseminated disease if left untreated is fatal
- infection more likely in middle-aged men (rapid dissemination can occur in women during pregnancy).
- median incubation period is 45 days following exposure to symptoms.
1. Primary Pulmonary Blastomycosis
- symptoms of disease (lungs) resembles tuberculosis, histoplasmosis, and bacterial infections
- inhalation of conidia
- may cause ARDS - adult respiratory distress syndrome
- pneumonia
- untreated disease is fatal
- lesions on the skin
- damage to the vertebrate, ribs, skull, and bones
- extensive and unresolving lung disease almost always goes systemic
- infected tissue in lung and other organs function as seed for other organ systems
- urogenital tract and central nervous system (gasterointestional involvement is rare)
- result of laboratory accidents
- accidental implantation during autopsy or while embalming patients that have died due to blastomycosis
- lesions usually on hands and fingers and these heal spontaneously without dissemination
Diagnosis
- disease must be differentiated form chronic granulomatous or suppurative pulmonary disease, such as histoplasmosis, tuberculosis, and bacterial diseases
- Blastomycosis can coexist with other lung infections.
- look at KOH preparation for presence of yeast phase
- hyphae rarely seen in diseased tissue
- yeast in B. dermatitidis resembles Histoplasma capsulatum except for presence of a braod-base of attachment between the bud and mother cell
- isolation and identification of fungus is best method for diagnosis of disease
- sputum and contaminated material mixed with an antibacterial antibiotics can be injected intraperitoneallly in mice, and these killed 3-4 weeks later to look for presence of pus and abscesses in the abdominal area.
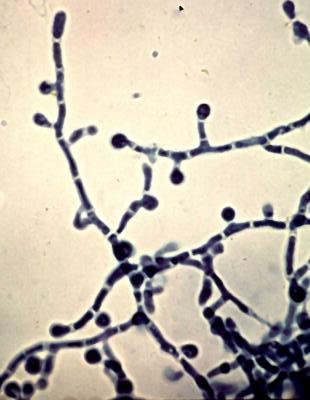
- mycelial form pretty much useless for purposes of identification. Cultures convert yeast phase at 37°C when grown on brain heart infusion or blood agar.
- amphotericin B (side effects, chills, fever, anorexia, headaches, nausea, vomiting, anemia, renal toxicity, (almost 100% effective if treatment started in time.)
- Experiments with imidazoles (e.g., miconazole, itraconazole, econazole, and ketoconazole) have shown modest success
- surgery may be useful but not until disease is under control
Refer to http://www.doctorfungus.org/thefungi/blastomyces.htm and http://www.mycolog.com/chapter23.htm for additional information and photographs.

- chronic disease
- primary pulmonary infection often inapparent
- disseminates to form ulcerative granulomata of the buccal (cheek and mouth), nasal and gastrointestinal mucosa.
- lymph nodes, cutaneous tissue or systemic involvement of multiple organ system.
- disease resembles blastomycosis and coccidioidomycosis
- geographically restricted to South and Central America
- the only etiologic agent is Paracoccidiodes brasilenensis
- in culture, conidiation is similar to Blastomyces dermatiditis; in tissue similar to Coccidioides immiits.
- once thought once to be rare, but skin tests reveal it to be subclinical and resolved infections common in endemic regions
- skin tests positives nearly equal between the sexes, but men between 20-50 years old are more likely to get clinically apparent paracoccidioidiomycosis
- source of infect may be soil but this has hot been conclusively demonstrated.
- Primary infection is PULMONARY, though infections of the mouth and alimentary canal suggested at one time source my have been from food, or from cleaning between teeth with grass and the trauma caused by this action.
I. Primary benign disease
- inapparent subclinical infection
- minor lung changes (bilateral lesions) and skin test reactivity seen in otherwise healthy people.
- Acute Form
- rare in adults
- rapid infection in lung and often fatal
- sometimes observed in immunosuppressed patients
- Progressive and chronic
pulmonary infections
- occurs in about 50% of cases
- respiratory insufficiency, dyspnea (difficulty breathing), fever, chest pain and cough productive of sputum.
- All lobes of the lung may be affected.
- Disseminated Disease (latent
and active)
- Mucocutaneous Lymphangitic Involvement
- primary infection is often subclinical\secondary involvement of the mouth region is most apparent present symptom
- lesions in the he mouth begin as papules or vesicles then ulcerate
- lesions are initially painless, extensive lesions cause distress during ingestion and chewing
- in advanced case the epiglottis and uvula are destroyed, hard palate is perforated, and lips and tongue may become involved.
- Gingival involvement may lead to tooth loss
- regional lymph nodes may become involved
- cutaneous infections usually extend form mouth infections
- mucocutaneous area is predisposed, possibly due to the cooling effect of air in this region which promotes growth of the fungus.
- Extracutaneous Disease
- foci for disease in organ systems without evidence of involvement from lungs or skin occur though uncommon (most common organ are the adrenal)
- Generalized Disease
- infrequent
- lymphatic system, spleen, intestine, adrenal, liver
- alimentary involvement results in abdominal pain, anorexia, diarrhea, and fever.
- rarely involved are the testes, brain , meninges, heart, large arteries, bones
- Mucocutaneous Lymphangitic Involvement
Differential Diagnosis
- imitates other mycoses and tuberculosis
- cases where paracoccidiomycosis and other lung diseases were present at the same time have been reported
- Often found in patients with other disease (malnutrition, ascariasis, etc.)
- sulfas - sulfamethoxypyridazine and sulfadimehtoxine 0.5 g following an initial dose of 1 g per day for one week - relapse is common.
- Amphotericin B and ketoconazole are equally effective in treating this disease.
- Laboratory Identification sputum, biopsy material and arterial from lesions and infected lymph nodes; cleared in 10 % KOH
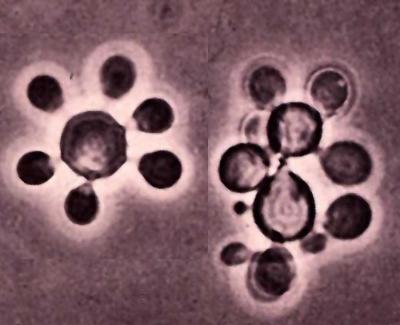
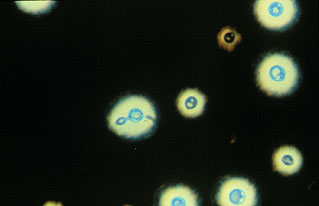
- yeasts are observed
- Cells vary in size depending on age 2-30 µm or more in diameter
- narrow point of attachment of buds to mother cell
- pattern of bud formation on mother cell varies, but often resembles a "Mickey Mouse" head or a pinwheel.
- Fungus isolated from contaminated materials at room temperature on medium (SDA) containing antibiotics (to kill contaminating bacteria) and cycloheximide (antifungal agent). If cultured at 37°C on medium (blood agar), antibiotics are added but not cycloheximide. Yeast phase is sensitive to cycloheximide (also true of Histoplasma and Blastomyces).
- Slow growing in culture.
- conidia of mycelia form are not characteristic so conversion to yeast phase is essential!
Refer to http://www.doctorfungus.org/mycoses/human/paracocci/paracoccidiomycosis.htm and http://botit.botany.wisc.edu/toms_fungi/jan2005.html for additional information and photographs.

HISTOPLASMOSIS - DARLING'S DISEASE
- worldwide; prevalent in eastern U. S.
- dimorphic fungus Histoplasma capsulatum
- infection through inhalation of conidia
- 95 % of cases are inapparent, subclinical, or completely benign
- diagnosed by x-rays through residual areas of pulmonary calcification and a positive histoplasmin skin test.
- chronic progressive lung disease, chronic cutaneous or systemic disease, or an acute fulminating, rapidly fatal, systemic infection.
- growth of fungus associate with guano and debris of
bat and birds, particularly due to the roosting habits of starlings.
-
Interesting Trivia: All the European Starlings in North America descended from 100 birds released in New York's Central Park in the early 1890s. A group dedicated to introducing America to all the birds mentioned in Shakespeare's works set the birds free. Today, European Starlings range from Alaska to Florida and northern Mexico, and their population is estimated at over 200 million birds (Source: http://www.birds.cornell.edu/AllAboutBirds/BirdGuide/European_Starling.html).

-
Photograph from http://www.inra.fr/hyppz/IMAGES/7033123.jpg
- teleomorph is Ajellomyces capsulatus, an ascomycete.
- disease described by Samuel Taylor Darling, 1905, in Panama (initial thought is was a protozoan).
- 1945 it was realized that the disease was common and widespread.
- In the U. S, estimated that 40,000,000 people have had the disease and 200,000 new infections arise every year.
- In culture at room temperature (below 35°C) on natural substrate, the fungus is filamentous
- white to brown in color pyriform to globose tuberculate macroconidia and small microconidia.
- the fungus favors guano-enriched environments with climate conidiation 68-90°F (22-29°C) and annual rainfall of 35-50 inches, relative humidity of 67-87% or more during the growing season.
- Chief vector of spores is wind.
- birds do not appear to be infected.
- bats may carry fungus via yeast-containing ulcers in the gut.
- Histoplasmin skin test - 21941 by Van Pernis filtrate of an asparagine glucose broth in which the mycelial stage has been growing for 2-4 months at 25°C. Histoplasmin infected intradermal as a 1:100 to 1:1000 dilution. Induration area seen after 48 hours indicates a positive skin test. In some parts of the U.S., by age 20, 80-90% of population show a positive skin test.
- Epidemics are anthropurgic - associated with human activity bulldozing, digging, etc.
- soils heavily infested can be treated by soaking it with a 3% formalin solution
Histoplasma capsulatum is a "true pathogenic" fungus sufficient quantity of microconidia will cause infection in the lungs of a healthy persons inhaled.
I. Benign Infection
- most people infections abort leaving calcifications in the lung (and spleen). Calcifications are sometimes a remnant of infection by other respiratory mycoses and tuberculosis, but less frequent.
- Resolution confers a certain amount of immunity and hypersensitivity to the antigenic components of the fungus; massive reinfection may result in a fatal acute allergic reaction
- Endemic Subclinical Disease
- 95% of histoplasmosis cases are asymptomatic
- Endemic Symptomatic Disease
- Ranges from mild to moderately severe - flu-like syndrome
- summer flu in children and "fungus flu" in adults
- Primary Cutaneous Histoplasmosis
- very rare
- usually a result of inadvertent infection of contaminated material (lab accidents, during an autopsy, bat guano)
- chancriform ulcer develops lesions heal spontaneously after several months.
- Endemic Histoplasmosis
- syndrome occurs when individuals are exposed to large quantities of conidia Primary infection symptoms don't appear for 10-18 days during which the organisms multiplies
- fever, malaise, chill, flu-like illness
- reinfection histoplasmosis symptoms develop in 3-7 days, on multiplication of organism. Flu-like symptoms.
A. Disseminated disease(defect in cellular immunity 50 out of 50,00 people infected each (1 in a 1000) chronic cavity disease (structural or anatomic defect predisposes to fungal colonization)
B. Chronic Pulmonary Histoplasmosis - associated with emphysema and exacerbated by smoking.
III. Aberrant fibrosis and hypersensitivity disease - encapsulation of fungus in a lesion. Fungus remains inactive but viable for years
A. Histoplasmoma - an enlarging fibrous mass (fibrous encapsulation and calcification) that develops around a healed primary focus of infection I the lung.
- Starts out 2-4 mm in size
- expands 1-2 mm annually reaching 3-4 cm over a 10 to 20 year period
- generally stops growing and calcifies completely (usually marble-sized)
- if surrounding structures are threatened surgical removal may be required
- fusion and excessive fibrosis in which the initial lesion is in one or several nodes in the mediastinum (i.e., septum that divides the pleural sacs containing all the thoracic viscera except the lungs)
- several nodes may become matted together, breakdown and becomes encapsulated to form a mass up to 10 cm in diameter.
- Mass is harmless, unless it impinges on vital adjacent structures including the superior vena cava, the pulmonary artery, the pulmonary veins and the bronchi.
- Histoplasmosis mimic tuberculosis, actinomycosis, viral and bacterial pneumonia, infectious mononucleosis, malaria and others.
- Therapy most infections resolve themselves
- often bed rest and supportive measures sufficient to effect resolution
- Amphotericin B is the drug of choice A total of 1-3 grams administered over a 1-2 month period - Side-effects are common and need to be monitored. In disseminated cases, 0.6 mg per Kg of body weight per day for six weeks.
- Ketoconazole has been curative in central nervous system disease at a dose of 200 mg per day.
- Sometimes... surgical excision of large cavities or granulomatous masses coupled with amphotericin B to prevent reactivation.
- Detect of organism in sputum by direct examination is difficult. KOH procedure is usually negative.
- Sputum, biopsied tissues, sternal puncture material staining after fixing 10 minutes in methanol on a slide and treated with Giemsa method of staining
- yeast cells are found in macrophage and monocytes (fungus is intracellular parasite)
- Isolation from disease tissue accomplished by growing on Blood Agar.
- Identification accomplished by demonstrating ability of fungus to convert at 37°C and the presence of tuberculate macroconidia in the filamentous s form grown at room temperature.
Refer to http://www.doctorfungus.org/mycoses/human/histo/histoplamosis_c.htm, http://www.mycolog.com/chapter23.htm, and http://botit.botany.wisc.edu/toms_fungi/jan2000.html for additional information and photographs.
Coccidioidomycosis
Coccidioidomycosis or "Valley Fever" is a benign, inapparent or mildly severe upper respiratory infection that usually resolves rapidly.
- Rarely, the disease is an acute or chronic severe disseminating, fatal mycosis.
- Recovery from the mild forms of the disease usually results in lifelong immunity to reinfection. Chronic pulmonary condition or as a systemic disease involving the meninges, bones, joints, subcutaneous and cutaneous tissues. Associated with these forms are the formation of burrowing abscesses.
- Etiologic agent of Coccidioidomycosis is Coccidioides immitis.
- This fungus is associated with a hot, semi-arid environment and is highly endemic to the southwestern U.S. and northern Mexico [LOWER SONORAN LIFE ZONE]. Endemic Foci are also found in Central America, Venezuela, Colombia, Paraguay, and Argentina.
- Most virulent of the fungal pathogens - working with live fungus requires the use of a biological safety cabinet or hood!
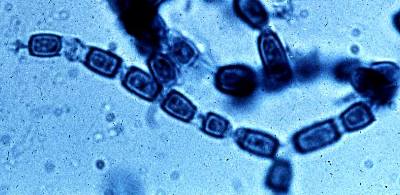
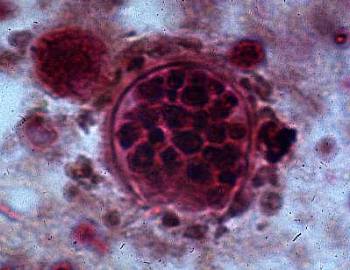
- Fungus is diphasic; In sputum or tissue, this fungus produces spherules which contain endospores. In culture the fungus produces cottony growth of mycelium and produces chains of arthrospores, which are barrel shaped. Mycelium grown at 37-40 C and increased levels of CO2 does not convert completely to a nonfilamentous form of growth - some spherules form.
- Identification often involves infecting experimental animals to observe spherules.
- Persons with pigmented skin appear to be more susceptible to the disease. The link is unclear. Statistically, male Filipinos and African Americans run the highest risk of contracting this disease.
- Coccidioidomycosis was the fist of the severe fatal mycoses in which an inapparent or mild form of disease was found to occur commonly in inhabitants of its endemic region.
- Probably a relatively new disease in humans. Endemic areas where it is found were very sparsely populated until the advent of European explorers and the subsequent settling agricultural and ranching populations in these regions. Indigenous populations that existed there, such as the Yokuts of the San Joaquin valley were eliminated by exposure the European diseases of influenza, cholera, syphilis, and smallpox. We do not know if coccidioidomycosis existed among them.
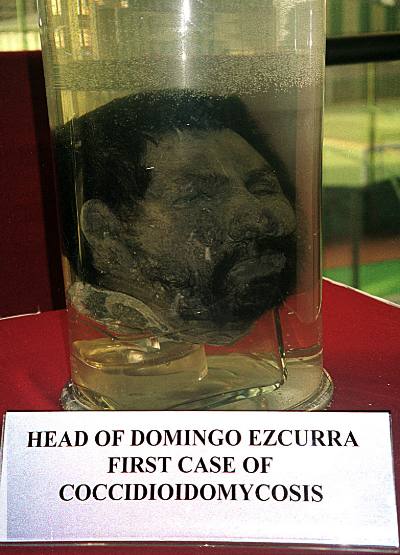
- Domingo Escurra, a soldier from the Argentine pampas, had recurrent tumors of the skin for fours years before entering the University hospital in Buenos Aires in 1891. His disease was studied by Alejandro Posadas, a student of the famous pathologist Rovert Wernicke. The patient lived another seven years during which time the investigators noted the progress and pathologic development of the disease. On examining lesions, they thought causal agent was an as yet undescribed protozoan in the order Coccidia. Posadas and Wernicke described the same patient in separated papers published (1892) in Argentina and Germany. In 1948, Dr. Flavio Niño found an unidentified head resembling that of the patient described by Posadas in the anatomy museum of the medical school Further study confirmed this was so, and therefore the specimens from the first case of coccidioidomycosis were rediscovered after being lost for half a century. This head and other appendages of the patient are now a featured exhibit of the medical school museum.
- First case of coccidioidomycosis first described by Emmet Rixford in San Joaquin Valley in 1886. Organism was named as Coccidioides immitis, but it was thought to be a protozoan. Early attempt to isolate the parasite were discarded because a mold developed, which at the time was thought to be a contaminant. Ophüla and Moffitt in 1900 described this organism as being a fungus.
- In 1932, Stewart and Meyer isolated C. immitis from soil in the San Joaquin Valley near a site where 4 Filipinos had contracted their severe or fatal infections. Site of infection and the presence in soil suggested strongly that portal of entry into the body was through the lungs.
- Myrnie Gifford working in San Joaquin Valley noted that patients with "valley fever or valley bumps" shared some symptoms and etiologic in common with severe infections caused by C. immitis. Dickson in 1937, coined the word "coccidioidomycosis", and by 1938, Dickson and Gifford concluded that Valley Fever were mild forms of coccidioidomycosis. The disease was not rare, instead it was rather frequent and common within the endemic area.
- Dickson, Gifford, and C. E. Smith began an extensive study of coccidioidomycosis in the San Joaquin alley. Smith criss-crossed the desert in an old Ford named the "Flying Chlamydospore".
- Smith developed and standardized the coccidioidin skin test. In the 1940's, airfields were built in endemic areas in the Valley. Smith formulated dust control methods, such as oiling roads, planting grass, and using swimming pools rather than dusty athletic files for recreation. The disease was discovered to be a problem in other areas of the American Southwest.
Refer to http://www.doctorfungus.org/mycoses/human/cocci/coccidioidomycosis.htm, http://www.mycolog.com/chapter23.htm, and http://botit.botany.wisc.edu/TOMS_FUNGI/jan2002.html for additional information and photographs.


OPPORTUNISTIC FUNGUS INFECTIONS
Opportunistic Fungus Infections are caused by organisms that are inherently of low virulence, and disease production depends on diminished host resistance to infection. Common etiologic agents of opportunistic infections are Aspergillus, Candida, Rhizopus, and Cryptococcus.
- very low inherent virulence.
- recovery from an infection does not establish a specific immunity , and reinfection may occur if general resistance is lowered again.
- there are no differences in susceptibility ascribable to age, sex, or race
- no transition is exhibited by organism in opportunistic fungus diseases. Fungus does not convert from one form to another.
LIST OF MAJOR ETIOLOGICAL OR CAUSAL AGENTS
Yeasts
- Candida spp.
- Cryptococcus spp.
Mycelial or Filamentous Fungi
- Zygomycetes - Mucor, Rhizopus, Conididiobolus, Basidiobolus
- Pseudallescheria boydii
- Aspergillus spp.
Protozoan-like fungi
- Pneumocystis carinii
Yeasts - unicellular fungal organisms that reproduce by budding and/or simple cell division and in the their anamorph stage belong to the form-class Blastomycetes.
- the term "yeast" has no taxonomic significance, because yeast species may belong to one of several different phyla, including Ascomycota, Basidiomycota or Deuteromycota
- in addition to being unicellular yeasts, may produce a mycelium or pseudomycelium
- all yeasts are opportunistic part of the natural mycota (endogenous and ubiquitous)
- one of the most common diseases of humans
- primary or secondary infection involving a member of the genus Candida
- clinical manifestations ranging from acute, subacute, chronic to episodic
- involvement localized as in the mouth, throat, nails, bronchi, lungs, or the gastrointestinal tract, or systemic as in septicemia, endocarditis and meningitis
- in the USA and Canada disease is called Candidiasis; common name in most other countries is Candidosis
- forms of candidiasis include thrush (mouth) and vaginitis (vagina)
- disease known since antiquity - thrush was recognized by Hippocrates in "Epidemics"
- 1841 (Berg) and 1844 (Bennett) demonstrated the fungal etiology of thrush
- Berg reproduced the disease in healthy babies by inoculating them
- in 1853, Robin recognized that thrush could become systemic
- vaginal candidiasis was described by Wilkinson (1849) in a 77-year old woman
- Haussmann in 1875, demonstrated that fungus of could be transmitted to the mouths of babies from lesions in the vagina. Haussmann also produced vaginitis in a healthy gravid female by inoculating Candida into her vagina
- other forms of candidiasis: subcutaneous, brain infection, intestinal disease, onychomycosis, cutaneous disease, endocarditis, and others were recognized over time by different people through 1940's.
- systemic and endocarditis that can be fatal often associated with broad-spectrum/antibacterial antibiotics and illegal drug use (heroin)
- most common cause is Candida albicans, but other species can cause it as well, C. krusei, C. tropicalis
- Extreme youth (resident mycota not yet established thrush, diaper rash)
- Physiological changes: pregnancy steroids, endocrine dysfunctions, diabetes
- Antibiotics therapy: these drugs wipe out microorganisms that keep resident species of Candida in check; in absence of competition, these yeasts flourish
- General debility and constitutional inadequacy: AIDS, immunosuppressive drugs
- Iatrogenic and barrier-break candidiasis insults due to catheters, surgery, self- administered injections by drugs users
- Some factors accelerate growth and colonization of
skin:
- damage to the skin
- moist skin (folded areas of the body, fruit picking, washing dishes), living in tropical environment, eating excessive fruit (sugars in gut)
- Candida albicans
- Candida albicans is a normal inhabitant of the alimentary tract and the mucocutaneous regions
- the normal skin possesses a resident yeast mycota but this does not include Candida albicans
- C. tropicalis
- C. krusei
- C. pseudotropicalis
- C. albicans var. stellatoida
- C. parapsilosis
- C. guilliermondii
- C. glabrata (Torulopsis glabrata)
A. Mucocutaneous involvement
1. Oral Candidiasis (thrush)
- patchy growths (which cause the peeling of membrane); appearance of milk curds as they crumble
- common in older people, diet deficiencies, premature babies, first sign of clinical AIDS
- Predisposing factors
- pregnant women (growth promoted by secretion of glycogen and progesterone)
- obesity
- diabetes (high sugar content in urine)
- may be sexually transmitted but rarely infects the penis (balanitis).
- Symptoms include puritis (itchiness), erythema (reddening of the skin), yellow milky discharge from he membranes, patches on membranes.
- difficult to diagnose because organism is common in most chronic lung conditions
- may be present in sputum without being in the lung
- look for quantity and frequency in diagnosis
- infection resides in the esophagus, intestine and anus.
- often associated with skin that is kept moist and where abrasions occur
- interdigital - between the fingers (occupational hazard of salad chefs, waiters, fruit canners, bartenders, etc.)
- groin, axillary regions (underarms), umbilicus (navel), feet and nails
- bacteria may be involved in a secondary invader
- nail infections - onychomycosis
- diaper rash may be caused by a species of Candida
1. Endocarditis - heart
- Predisposing conditions:
- drug addicts using unclean needles
- preexisting valvular disease
- people treated with antibiotics
- intravenous infusion = gets into tubes of machine
- In one study - 59 cases were species of Candida found after heart surgery - only 6 patients survived.
- Bladder and kidney included
- more common in women then men
- yeast can be found in urine with no obvious infection present
- about half of the patients based on one study, who died after renal transplant died from systemic fungal infections; ½ of these were due to Candida infections
- relatively rare, probably disseminated from another part of the body that is infected
- in blood and potentially fatal patients often predisposed through antibiotic therapy or a result of having leukemia
- Candidids - similar to the dermatophytid reaction caused by dermatophytes
- Eczema (reddening and itching of skin, may become crusty and scaly)
- Gastritis
- because the infections are opportunistic it is important to control the predisposing factors
- nystatin -first polyene antimycotic discovered
- Hazen and Brown (two women discovered this in New York) profits turned over to Research Institute for the study of Fungal Disease. Trade Name - Mycostatin
- produced by Streptomyces noursei
- insoluble in water, side effects not pronounced; sensitivity may develop to antibiotics
- organism do not develop resistance (rare)
- topical application or given orally as tablets for gastrointestinal infections
- heat instable and oxidizes in light
- fungistatic, not fungicidal
- ketoconazole taken orally can improve chronic mucocutaneous infections
- amphotericin B is sometimes effective in systemic disease but resistance may develop
- Diflucan (Fluconazole) - from Pfizer. Contains prescribing information.
- Serological tests are not reliable in identifying organisms or disease
- Colonies and cultures are unpigmented (unlike
Rhodotorula rubra)
- no capsule (unlike Cryptococcus)
- pseudomycelium caused by elongating yeast cells.
- blastospores (numerous budding cells) from pseudomycelium or yeast cells
- chlamydospores are located on the terminal end of the pseudohyphae. Spores various in sized (8-12 mm)
- Carbohydrate assimilation tests or diagnostic kits (e.g., Analytical Profile Index [API 20C] Yeast Identification Kit by bioMerieux Vitek, Inc.)
Refer to http://www.doctorfungus.org/mycoses/human/Candida/Candida_index.htm, http://www.mycolog.com/chapter23.htm, and http://botit.botany.wisc.edu/toms_fungi/jan99.html for additional information and photographs.



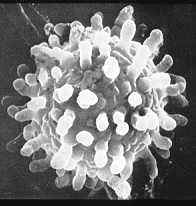
- disease caused by Cryptococcus neoformans
- the only basidiomycete that is known to be a pathogen on humans
- fungus is found in soil, fruits, milk, bovine mastitis, and pigeon droppings
- typically associated with pigeon roosts and guano
- alkaline, high-nitrogen, high-salt substrate.
- like Coccidioides immitis, C. neoformans appears unable to survive or compete with other species in other situations. Cryptococci disappear from infected debris when it is mixed with soil. Eaten by amoebas (Acanthamoeba species)
- Filobasidiella neoformans represents the teleomorph
- Cryptococcus neoformams var. neoformans (serotype A and D) and C. neoformans var. gattii (serotype B and C)
- C. albidus and a few other species have been isolated on rare occasions from infected patients
- Rhoda Benham clearly differentiated blastomycosis from cryptococcosis in 1934. She showed that cutaneous European type of cryptococcosis was caused by the same organism that produces the meningitic form more commonly reported in America.
- pulmonary infection, rarely enters through direct inoculation by implantation (usually enters body through lungs)
- usually causes a mild, transitory infection that is self-healing (like histoplasmosis) - common disease
- no good skin test to tell if you have had the disease
- predisposing conditions include: severely immunocompromised individuals (organ transplant recipients, AIDS), collagen diseases (lupus erythematosus), drug abuse, endogenous and exogenous debilitating conditions (Cushing's syndrome)
- disease can become chronic and last for years.
- often Cryptococcosis is the first symptom of AIDS, emphasizing this disease as malade signal or signal disease!
- if fungus disseminates, gets into CNS (sudden and severe meningitis)
- fungus has a predilection for the CNS, why? Fewer inhibitory substances in serum, less likely to be attacked by macrophage, and nitrogen and carbon source in fluids encourages growth.
- Typical signs of invasion of CNS are severe headache and fever.
- Before advent of drug therapy, this form, almost always fatal. Amphotericin B along with 5-fluorocytosine has cut mortality to about 6 %
- When it disseminates can also appear on skin, in bones, and other organs. Skin lesions, if severe, can ulcerate. Commonly confused with blastomycosis. The term blastomycosis has been used very loosely to designate any infection in which a budding yeast cell was found.
- mount using India ink (carbon-based ink) for best view of capsule.
- rare to see a pseudomycelium
- do not use cyclohexamide for isolation (some strains are inhibited by as little as 1 ppm)
- another way to see capsule, inject into mouse interperitoneally and look at peritoneal fluid
- India ink method (useful for visualizing the organisms in macerated biopsy material, centrifuged sediment of spinal fluid, cisternal fluid, urine, or touch slides of autopsy materials).
- use very little ink so can see capsule
- ink will not penetrate capsule, so see a clear area which is the capsule
- ink will not kill fungus, so dispose of slides properly (STERILIZE!)
- advisable to run a saline control slide, since India ink can become contaminated with microorganisms or ink may change in quality over time
- ink particles can be seen bouncing around due to Brownian movement
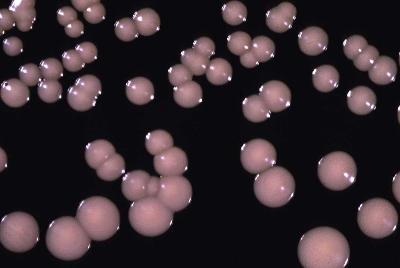
- in culture, Cryptococcus is similar to Candida except culture tends to be gooey or slimy and falls to bottom of culture tube
- Physiological differentiation, especially between species of Cryptococcus is a common practice.
- Chemotherapy - amphotericin B (approx. 75 % effective).
- 5-flourocytosine (approx. 40 % effective, used mainly as a back up drug - inhibits protein synthesis).
- Garlic has been shown to be noted to be active against Cryptococcus. An extract has been used as an oral and intramuscular agent in patients with cryptoccocal meningitis.
- Forms of cryptoccocal infection have been found in horse, dog, fox, cat, dolphin, cheetah, civet, monkey, guinea pig, ferret, various birds, and dairy cattle.
Refer to http://www.doctorfungus.org/mycoses/human/crypto/crypto_index.htm, http://www.uphs.upenn.edu/bugdrug/antibiotic_manual/Gram5.htm, and http://en.wikipedia.org/wiki/Cryptococcus_neoformans.

Mycelial Fungi - opportunistic pathogens that do not convert from a filamentous form to another phase of growth (e.g., yeast phase) when pathogenesis occurs.
Zygomycosis
- the term "zygomycosis" encompasses any human or
animal disease in which the etiologic agent is a member of the Phylum
Zygomycota
- Hyphae are non septate and coenocytic (i.e., non-septate - no cross-walls).
- Cell walls contain chitin, chitosan, and polyglucuronic acid.
- Flagellated spores are absent.
- Reproduce asexually by producing sporangiospores within a special sac called the sporangium.
- Sexual spores are called zygospore(s) contained within a zygosporangium
- Visit: http://tolweb.org/tree?group=Zygomycota
- http://faculty.baruch.cuny.edu/jwahlert/bio1003/fungi.html
- http://www.kcom.edu/faculty/chamberlain/Website/LECTS/Fungi.htm#sup
- http://tolweb.org/tree?group=Zygomycota
PHYLUM ZYGOMYCOTA


Source of Rhizopus photographs and other information on zygomycetes: - in humans, disease is manifested in highly stressed
or debilitated individuals
- metabolic acidosis
- immunosuppression
- trauma
- in animals and some cases in humans, disease is manifested after exposure to large quantities of a particular fungi or spores (e.g., contaminated feed, aerosols of fungal spores).
- Phycomycosis and mucormycosis are older names that refer to diseases caused by phycomycetes (obsolete taxonomic designation which included the zygomycetes, oomycetes, and chytrids). Mucormycosis referred to diseases caused by members of the Order Mucorales in the Zygomycetes.
- Entomophthoromycosis Conidiobolae is synonymous with rhinofacial zygomycosis caused by Conidiobolus coronatus (see http://www.mycology.adelaide.edu.au/gallery/photos/conidio7.html) which is also a parasite of insects and associated with decaying plant debris.
- Entomophthoromycosis Basidiobolae is a chronic subcutaneous form of zygomycosis caused by Basidiobolus ranarum or B. haptosporus. Fungus is common on decaying vegetation, soil and in the excrement of frogs.
- General forms of Zygomycosis
- most acute and rapidly fatal fungal disease
- some patients die within one week after the onset of symptoms
- death rate was about 90%, but now it is about 50 %
- uncontrolled diabetes with acidosis, acidosis caused by excessive aspirin intake, diarrhea, uremia, or leukemia, lymphoma, severe burns, and other diseases
- incidence of zygomycosis is on the increase due to immunosuppressant drugs, cortisone (steroids), and other drugs
- Etiologic agents include: Rhizopus arrhizus and other species; Absidia corymbifera, Mucor spp., and Mortierella spp.
1. Rhinocerebral - most common form, associated with uncontrolled diabetes.
- nasal and orbital infection
- encephalitis
- invasion of larger blood vessels and arteries
- patient may go into coma and die
- Mark Tatum of Kentucky (seen below; after surgery, with and without facial prosthetic) survived from rhinocerebral zygomycosis in 2000. Surgery was required to remove infected tissue. He died five years later on February 26, 2005.


- surgery is necessary to save the patient - often fatal if not treated
- heart may become invaded.
- symptoms of abdominal zygomycosis vary and depend on the site and extent of involvement. Nonspecific abdominal pain, atypical peptic ulcer, diarrhea, "coffee ground" hematemesis (regarding blood), and bloody stools are recorded
- if patient dies and disease recognized upon autopsy, with ulceration of gastric mucosa with thrombosis (blood clotting) and associated vessels.
- malnutrition, typhoid fever, amebic colitis.
- may include liver, pancreas and spleen.
- In autopsy - in tissue, wide non-septate hyphae
- 1950's Duke Univer. Med Center first isolated a Rhizopus and determined it as the etiologic agent. Patient was treated and survived.
- Over 150 cases reported; Central and West Africa, Colombia, Brazil and the Caribbean.
- Animal infections, are reported in the U.S., Australia and other diverse parts of the world.
- Treatment with involves use of amphotericin B, sulfa, surgery, iodides. Some cases heal spontaneously.
- Refer to
http://www.doctorfungus.org/thefungi/Conidiobolus.htm,
http://www.mold-help.org/index.php?option=content&task=view&id=473,
http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0036-46652001000400012&lng=es&nrm=&tlng=en,
and
http://www.mycology.adelaide.edu.au/gallery/photos/conidio2.html for
additional information.

- 250+ cases of this disease have been recorded. Most cases have been from Uganda, Nigeria, and Indonesia, with a scattering of cases in India, Costa Rica, Togo the Near East, Brazil, and a few reports in the United States
- Portal of entry unknown perhaps insect or mosquito bites.
- Basidiobolus ranarum is
associated with the dung of frogs and represents a saprophyte.
- Sporangia (AKA conidia) are forcibly discharge. Turgor pressure created by contraction of the elastic sporangiophore wall causes a tear in the sporangial wall lifting the sporangium away from the dung. The sporangium and "skirt" travel about 0.5 cm. The skirt detaches from the sporangium and the sporangium continues to travel an additional distance of 1-2 cm. This form of explosive "spore" dispersal has been referred to as a "two stage rocket" form of propulsion created by the rushing of fluid out of the expelled skirt. Momentum carries the sporangium the remaining distance.
- This fungus also produces sporangioles (also called capilliconidia with haptor) which are sticky and catch onto passing insects, like beetles. The fungus is thought to re-enter the amphibian or reptiles digestive track when the animal eats a tainted beetle. In the stomach the capilliconidia cleaves into a number of spores. Upon voiding their excrement, the fungus mycelium grows and produces more sporangia (AKA conidia) and sporangioles (AKA capilliconidia).
- Disease is called Entomophthoromycosis Basidiobolae (a form of zygomycosis in humans in which tumor like enlargements develop in the subcutaneous tissue) was once thought to be caused by a species other than Basidiobolus ranarum (called Basidiobolus haptosporus). However isolates obtained from infected tissues in humans appears to be B. ranarum and not a distinct separate species.
- Basidiobolus: Dispersal of the explosive dispersal of the sporangium; the two stage rocket.
- Refer to http://www.doctorfungus.org/thefungi/Basidiobolus.htm, http://www.mycology.adelaide.edu.au/gallery/photos/basidiobolus01.html, and http://www.mycology.adelaide.edu.au/Mycoses/Subcutaneous/Zygomycosis/index.html for additional information.

- Burned patients, trauma to skin (wound, catheter), surgery, contaminated bandages.
- Amphotericin B is fungistatic but successful in some reported cases.
- Pathogens show variable sensitivity to imidazoles.
- not necessarily effective
- control the diabetes
- control condition which predispose the person to the disease
- drug of choice is amphotericin B and/or KI
- look at scrapings and look at long nonseptate hyphae
- biopsy
- aspirated material
- sputum
- If you are attempting to culture do not incorporate cyclohexamide into the medium. Fungus is sensitive to this fungicide!
- Cultures grow very fast! Aerial mycelia, and may fill up plate within 4 or 5 days.
Refer to http://www.doctorfungus.org/mycoses/human/zygo/zygomycosis.htm and http://www.mycolog.com/chapter23.htm for additional information and photographs.

Pseudallescheria boydii - soil/water inhabiting fungus with worldwide distribution
- caused by Pseudallescheria boydii - soil/water inhabiting fungus with worldwide distribution
- low virulencePseudallescheria boydii - soil/water inhabiting fungus with worldwide distribution
- opportunistic fungus
- usually associated with Immunosuppressive drugs, underlying disease, trauma, barrier breaks, disease, aspiration of soil, swamp or sewer water (in drowning victims)
- pulmonary colonization (lungs)
- Pseudallescheria arthritis and osteomyelitis (inflammation of the bone marrow).
- fungoma
- invasive pneumonitis
- mycotic keratitis (fungus infection of the cornea)
- endophthalmitis - inner eye infections
- endocarditis - inflammation of the endocardium (membranes that line the cavities of the heart)
- meningitis - infection of the meninges investing the spinal cord and the brain
- brain abscesses
- sinusitis - inflammation of the sinuses
- cutaneous and subcutaneous infection
- mycotic mycetoma - usually more common in men (3:1 to 5:1) than in women.
- Infection more common in ages 20-40.
- Chronic otitis (ear infection) almost always with children. Chronic infection sometimes lethal
Refer to http://www.mycology.adelaide.edu.au/Mycoses/Opportunistic/Pseudallescheriasis_and_Scedosporium_infection/index.html and http://www.doctorfungus.org/thefungi/pseudallescheria.htm for additional information and photographs.
MYCOTIC MYCETOMA - accounts for 99 % of infections- usually results from trauma or puncture wounds to feet, legs, arms and hands (usually on the feet)
- starts out as tumor-like to subcutaneous swelling
- ruptures near the surface; infects deeper tissues including subcutaneous tissues and ligaments (tendons, muscles and bone are usually spared)
- small particles or grains leak out of the lesions - these represent the to yellowish microcolonies
- lesions of mycetoma seldom heal spontaneously
- disease is chronic may continue for 40-50 years
- P. boydii is resistant to all systemically useful drugs, including amphotericin B, KI, 5-fluorocytosine, 2-hydroxystilbamidine
- ketoconazole appears to be ineffective in clinical trials
- intravenous miconazole (9 mg per Kg of body weight sometimes higher doses) shows promise
- surgery and removal of tumor ( if small it is encapsulate, if larger amputation my be required)
- Combining miconazole and surgery may prove useful in effectively treating the disease.
- Lung and upper respiratory tract
- fungoma (fungus ball formation - similar to Aspergillus fungoma and difficult to distinguish)
- conidia are often formed in tissue
- predisposing condition usually some preformed cavity or cyst
- surgery usually curative
- most lower respiratory tract infections lead to pneumonia - which is likely to fatal, but person generally compromised (e.g. taking steroids, AIDS etc.)
- miconazole, amphotericin B and surgery are recommended forms of drug treatments.
- P. boydii less common cause of cornea infections than Aspergillus spp. and Fusarium spp.
- associated with injury to eye, such as plant debris, splinters, twigs, (fish scale in one fishery worker)
- amphotericin B, pimaricin, nystatin can cure disease in some instances.
- most infections occur in compromised patients and similar infections can also be caused by Candida species
- penetrating trauma or surgery (exogenous) or endogenous (from some other point with the body - e.g., from the brain).
CULTURE OF THE ETIOLOGIC AGENT
- Grows readily on Sabouraud's Dextrose Agar but my not produce cleistothecia on rich media
- repeated transfers to deficient media induces ascocarp formation
- Pseudallescheria boydii is homothallic (self-fertile) and represents the teleomorph (an Ascomycete)
- The anamorph is Scedosporium apiospermum and S. inflatum
- In older cultures, "house mouse" gray mycelium
- Asexual conidia produce annellocondia (single) or wet clusters of conidia called Graphium-type of conidiation "synnemata".
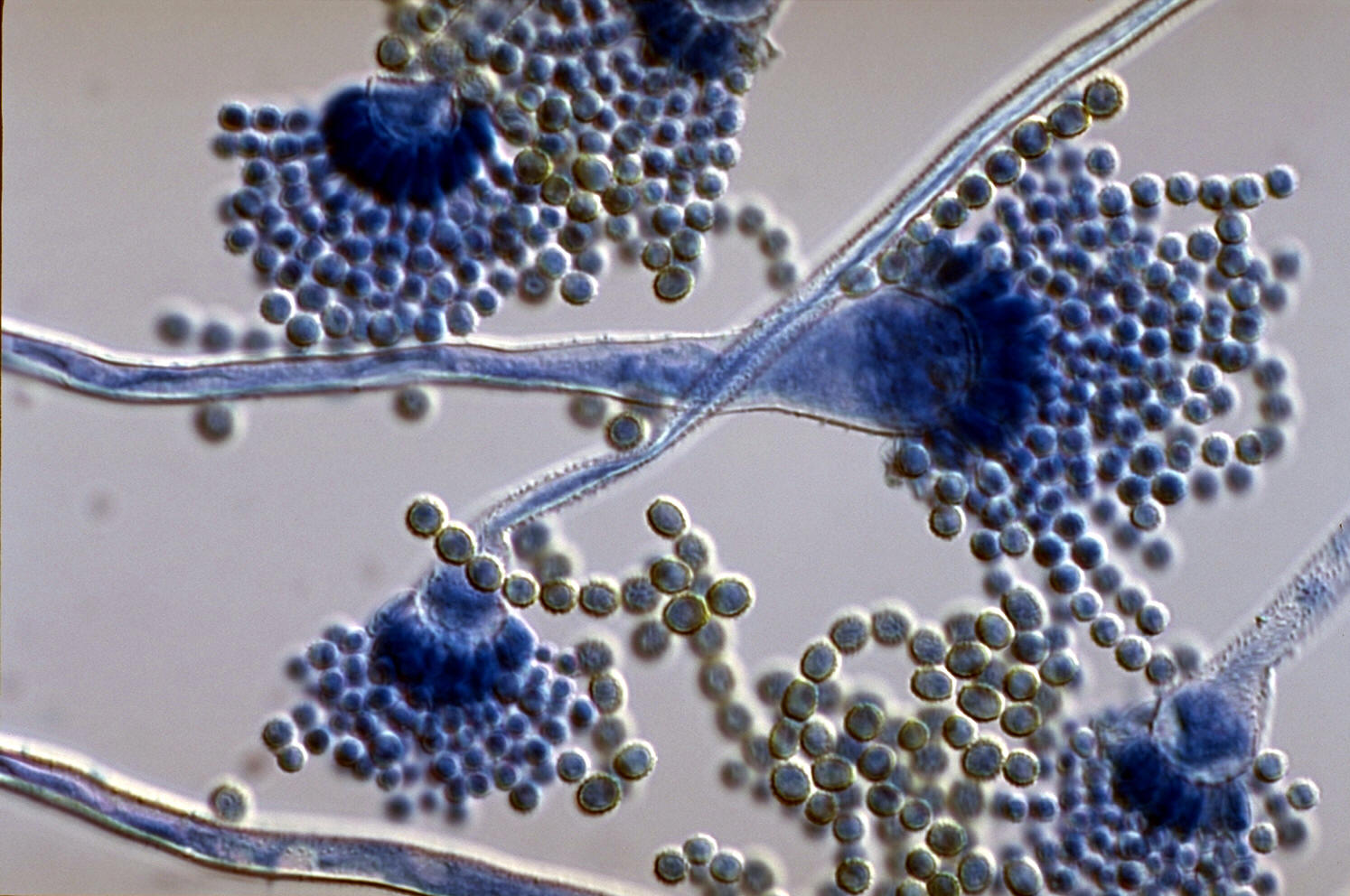
- caused by species of Aspergillus.
- Visit: http://www.pfdb.net/photo/mirhendi_h/box020909/standard/a_flavus_s.jpg for source of following photograph of Aspergillus flavus:
- disease discovered in the lungs of a jay - 1815, originally thought to be disease of birds
- penguins in London zoo began dying from Aspergillosis. Birds are susceptible, because this fungus is somewhat thermophilic (heat-loving)
- mycotic abortion of sheep and cattle, pulmonary infections of birds, and toxicosis due to ingest of grain containing fugal by-products
- first recognized as a human disease in 1842
- in humans, Aspergillosis is more prevent in males than females or children
- "aspergillosis" refers to a spectrum of human disease which include, otomycosis (ear), mycotic keratitis (eye), rarely mycetoma, cutaneous infection, pulmonary infection, allergy, systemic and fatal disseminated disease
- Many cases of aspergillosis coexisting with some other debilitating disease.
- Aspergillus fumigatus
- A. niger
- A. flavus (produces aflatoxin - most potent carcinogen known, Turkey-X disease - 1960, it was later discovered that contaminate peanut meal fed to poultry was the culprit).
- A. amstelodami - grow under condition of low water and this produces cleistothecia (indicating that it is an ascomycete).
- Invades lungs and bronchi - symptoms similar to TB
- necrosis, and inflammation and granules in the lung tissue
- fungal growth in lung is mycelial
- Aspergillus spp. can be secondary invaders of any other lung disease
- fungus can be found in sputum (Hyphae or spores)
- sometimes grows in cavities left by Cocci, Histo, and other lung diseases
- spores may form in cavities and bronchi of lung
- found in agricultural workers, fur-cleaners, pigeon breeders (feed squabs with mouth-eaten feed)
- Aspergilloma - "fungus ball", not found infrequently.
- occurs in bronchi and causes blockage in the lung
- fungi growing in secretions of lung
- Farmer's lung" - may involve thermophilic actinomycete and/or Aspergillus. Extreme allergic reaction, acute or chronic sensitization, sometimes fatal. A strong asthmatic reaction to these function - occupational hazard around moldy grain or dirty air filters
- in addition symptoms include, chill and fever, abnormalities in lung
- shallow breathing, livid lips, weakness, and a chronic cough
- disseminated form from a primary lung infection ==> gets through the blood system or lymphatic system, may cause infection in the heart (endocarditis), meninges, rarely bones or gastrointestinal involvement
- generally fatal, especially in children
- been known to enter patients who are undergoing dialysis.
- the orbit of the eye, in the conjunctive, eyeball, or nasal sinuses
- Otomycosis (ear)
- nail infection - onychomycosis.
- Aspergillin Skin Tests -95% of the people with allergic rxns, 22% with fungus balls.
- immunodiffusion tests are useful in identifying that the patient is producing antibodies to fungus.
- difficult to identify the common saprophyte as the cause of disease.
- Pulmonary form ==> KI is taken orally, or NaI intravenously.
- Amphotericin B is not always successful but is used for systemic forms of this disease.
- Nystatin is useful in pulmonary forms, by inhalation and used for localized forms that occur in the sinuses
- Allergic aspergillosis, treat the infection and hypersensitivity
- Prednisone and other steroids are used during the acute phase, but precautioned in chronic cases. Reduce symptoms of bronchial plugging by mucus containing the fungus. Vigorous physiotherapy, bronchoscopic aspiration, and lavage are recommended
- with Aspergillomas - fungus balls are removed surgically
Pneumocytis carinii Pneumonia (PCP)
- THE FOLLOWING INFORMATION ON PNEUMOCYTIS WAS GLEANED FROM THE TEXTBOOK "INTRODUCTORY MYCOLOGY", BY C. J. ALEXOPOULOS, C. W. MIMS, AND M. BLACKWELL, 1996. JOHN WILEY & SONS, NEW YORK, 868 PAGES.
- causal agent is Pneumocystis carinii which results in a virulent pneumonia in immunocompromised humans, primarily those infected with HIV
- extracellular parasite of a number of mammals, including human beings, rats, mice, ferrets, horses, pigs, and rabbits
- the fungus binds to epithelial cells of the alveoli, and in addition to a lung infection, it may become disseminated to other organs and throughout the bone marrow
- pathogen first described as a protozoan from lungs of rats in France in 1912
- recognized in humans much later (1942)
- first found in individuals who were severely malnourished or immunocompromised after drug therapy, it was only after the spread of HIV that the organism became widely known
- recognition of Pneumocystis as a fungus is more recent occurrence
- fungus probably related to yeast-like ascomycetes (sensitive to antimycotic benomyl, as are other ascomycetes and deuteromycetes)
- Ultrastructural studies of spores using electron microscopy, observation of ascomycete-like synaptonemal complexes formed during meiosis and DNA sequences suggest that this organism is a fungus, and not a protozoan.
- Although the evidence currently supports that Pneumocystis carinii is an early diverging ascomycete, the matter is not completely settled.
- Pneumonocystis has not been grown in culture
- This fungus is probably air dispersed; however, dispersal has not been observed and the dispersal stage is not known.
- Pneumocystis carinii (photograph and information)
- http://www.doctorfungus.org/thefungi/pneumocystis.htm
- Childhood Infections (Pneumocystis carinii)
This web page is organized and maintained by M. Huss. Last updated 10-19-08.