MUSHROOM TOXINS AND POISONINGS - Refer to the following notes, your textbook and the following internet link for more information - Mushroom Poisoning.
1. AMATOXINS: Amanitin (cyclic octapeptides)
Galerina autumnalis and Amanita phalloides (the death cap), A. verna and A. virosa (the destroying angel).
phallotoxins - if injected into mice, death at high doses occurs in 1 hour. Ten times more lethal than cyanide! However, it is not easily absorbed by digestive system if ingested.
amatoxins - if injected into a mouse, lethal effects are not exerted for 15 hours. Lethal dose for an adult human is 5-10 mg. Inhibits RNA polymerase, so it interferes with RNA transcription, which results in a slow lingering death.
Stages of Illness
Phase 1 - Latency or lag period of 10-12 hours, while toxins are absorbed through digestive system and begin to attack the kidneys and liver.
Phase 2 - Gastrointestinal phase. Onset of symptoms: severe abdominal pains, nausea, vomiting, diarrhea, delirium, hallucinations, hypoglycemia, life-threatening dehydration.
Phase 3 - Severe gastrointestinal phase wanes, brief remission of symptoms after 3-4 days. Jaundice sets in, renal disturbances, toxic hepatitis, liver enlarges, hemorrhaging of liver.
Phase 4 - Death takes place within 6-8 days after ingestion due to liver and renal failure, cardiac damage.
Treatment
No known antidote. Immediate evacuation of gastrointestinal tract, fluids, hemodialysis, slurry of activated charcoal, supportive measures, and if all else fails, administer a liver transplant.
Thioctic acid in glucose delivered intravenously is recommended by some experts.
Bastien treatment: vitamin C, nifuroxazide and dihydrostreptomycin, fluids, electrolytes, and penicillin. Dr. Bastien has treated himself twice after having eaten A. phalloides on two separate occasions. He survived the experience.
1. The genus Amanita is characterized by having a membranous annulus (remnant of the partial veil) and a cup-like volva (remnant of a universal veil). White gills and white spore print. The mushrooms cap may be white or colored depending on the species.
2. Meixner test can help determine whether a particular mushroom
contains amatoxins. The stalk or cap is pressed to a piece of newsprint or
other crude paper containing lignin. The area is allowed to dry and drop
of concentrated hydrochloric acid is added. If a blue color appear in 5-10
minutes, amatoxins are assumed to be present. This procedure appears to
involve an acid-catalyzed reaction of the lignin in the paper with the amatoxins.
2. HYDRAZINES: Gyromitrin, monmethylhydrazine (MMH)
False morels, species of Gyromitra and Helvella species cause poisonings. Hydrolyzed gyromitrin produces MMH, rocket fuel, which is very toxic. This toxin causes hemolysis of red blood cells. Patients suffer from faintness, loss of muscular control, and fever. In severe cases, jaundice and convulsions occur, and coma and death may ensue after 2-7 days. Parboiling (avoid breathing steam) of mushrooms can remove toxin. Also there appears to be a threshold of toxicity, many people have "an all or nothing response". According to Dr. Orson K. Miller Jr. (pers. comm.), this or some other toxin in these mushrooms have been shown to induce tumors in laboratory animals - therefore potentially carcinogenic in humans.
Treatment: Little point in evacuating the
gut unless poisoning is suspected right after ingestion. Pyridoxine
hydrochloride should be administered as a specific physiological antagonist to
MMH. Blood sugar, liver and kidney function, and free hemoglobin level
should be monitored. Intravenous glucose, forced diuresis (to remove the
free hemoglobin), if free hemoglobin levels increase, hemodialysis (circulating
the blood through a semipermeable membrane in an isotonic medium) in severer
cases, and other supportive measures as needed.
3. ORELLANINE
Orellanine is a deadly poison found in some species of the genus Cortinarius. Orellanine is a bipyridine, as is the herbicide paraquat. Orellanine inhibits the activity of the enzyme alkaline phosphatase in kidney cells.
Symptoms are similar to poisoning induced by amatoxins, but muscular pain,
excessive thirst, and painful urination may appear after 36 hours but be delayed
as long as one to two weeks after ingestion. Orellanine destroys the
kidney tubules and in severe cases, treatment may require blood dialysis or
kidney transplant. Fatalities occur, orellanine poisoning should be
considered in cases when kidney failure occurs from an unknown cause.
Toxic cyclopeptides called cortinarins may also be present and play a role in Cortinarius
poisonings. There may be as many as 800 species of Cortinarius in
North America, all of which should be excluded from the dinning table.
Mushrooms produced by members of the genus Cortinarius
are characterized by possessing a cobweb like cortina (remnant of the partial
veil covering the gills).
1. COPRINE (Antabuse-like - disulfiram-like poisoning)
Toxin found in Coprinus spp. (C. atramentarius). Toxin binds to molybdenum and blocks acetaldehyde dehydrogenase and arrests ethanol metabolism. Actually this is acetaldehyde poisoning. Symptoms begin ½ to 1 hour after drinking alcohol is taken in 4 to 5 days after eating mushrooms or along with mushrooms.
Flushing of the neck and face. Metallic taste in mouth, tingling sensations in the limbs, numbness in the hands, headache, throbbing of the neck veins. Chest pains, nausea, sweating, vomiting. Recovery usually occurs with several hours.
2. MUSCARINE
Amanita
muscaria - the fly agaric, contains muscarine (an amine), also found in Clitocybe
and Inocybe
(little white and brown mushrooms). PSL syndrome = perspiration, salivation and
lachrymation. Latent period of 30 minutes up to six hours before symptoms
appear. Toxin stimulates the exocrine glands (producers of sweat, saliva
and tears). Symptoms also include: salivation, nausea, vomiting, abdominal
pains, thirst, bloody stools, rapid then slow respiration, loss of
consciousness, delirium, hallucinations, manic condition and stupor. In
severe cases, convulsions and death (about 1% of cases). Primary
danger of toxin is that heart may stop, but this is rare. Atropine is
carefully administered to compensate for symptoms.
1. IBOTENIC ACID-MUSCIMOL
Amanita muscaria when fresh contains ibotenic acid. This converts to muscimol when mushrooms are dried out. For this reason dried mushrooms are more potent than fresh ones. Muscle spasms, dizziness, vomiting, followed by a deep sleep full of fantastic dreams. Substance responsible effects the central nervous system, and creates the feeling of elation and an altered perception of reality. The effects of this mushroom have been know since antiquity. Siberian tribes used this as a religious and recreational intoxicant. The active principle collects in the urine, and drinking the urine was a way to recycle the inebriant.
Few deaths are associated with this type of poisoning, 10 or more mushrooms can constitute a fatal dose. Recovery is usually spontaneous and within 24 hours. Atropine should not be given, it may exacerbate the condition.
2. PSILOCYBIN-PSILOCIN
Hallucinogenic mushrooms used by Aztecs of Mexico and Central American Indians. "Magic mushrooms" include Psilocybe, Panaelous, Conocybe, and Gymnopilus. Altered states of reality, hallucinations, feelings of euphoria, etc...
Psilocybin and psilocin are the psychoactive compounds.
Hydroxytryptamine derivatives related to serotonin. Average effective dose
of psilocybin is 4-8 mg, equal to about 2 g of dried mushrooms. Bad trips
are possible but poisoning is unlikely unless excessive overdose. Hallucinations
may be suppressed by chlorpromazine, and convulsions by diazepam.
MISCELLANEOUS OR UNCHARACTERIZED TOXINS
A wide variety of undetermined toxins associated with wild mushrooms.
Ingestion causes gastrointestinal distress (nausea, vomiting, diarrhea,
abdominal cramps) after about 30 to 90 minutes of being eaten. Symptoms
generally clear up spontaneously in 3-4 hours, and completed recovery takes only
a day or so. Treatment includes emptying the stomach, monitoring for
dehydration, reduced blood pressure or impaired kidney function. Chlorophyllum
molybdites (see Tom
Volk's Fungi) is a common cause in this country.
FINALLY, MUSHROOMS CAN CAUSE ILLNESS...
1. Ingestion of edible mushrooms that are rotting or contaminated with pathogenic bacteria, heavy metals, or toxic chemicals. It is best not to collect and ingest edible mushrooms growing along roadways or highways (these may accumulate significant levels of lead or other toxic organic substances).
2. Ingestion of edible wild mushrooms that cause an idiosyncratic reaction in a particular individual (i.e., a physiological or temperamental peculiarity). Symptoms may include an allergic response or gastrointestinal irritation or upset.
3. Ingestion of edible wild mushrooms that causes a person to become overly concerned or worried, leading to an anxiety reaction or psychosomatic illness. Miscellaneous symptoms include among others, nausea, vomiting, panic reaction, chills, hot flashes, sweaty palms on the hands, etc. Treatment: Reassurance and/or diazepam.
4. Deliberate inhalation of spores - one case involved campers that thought inhalation of puffball spores would get them high. Sent a group of people to the emergency room unable to breath. Two individuals got secondary respiratory infections and almost died.
5. Excessive ingestion of certain edible fungi, like puffballs, can lead to a bulk laxative effect. Not harmful but it may be a bit disconcerting to the individual experiencing this phenomenon.
The following is a compilation of mycotoxins and fungi that pose a health hazard to animals and humans that consume contaminated foodstuffs. However you should be aware that this page lists only some of the major types of toxicoses caused by the secondary metabolites of fungi, and therefore is incomplete.
Fusarium toxins - produced by several species.
-
Zearalenones (produced in molded maize)
- Toxic to swine and causes abnormalities and degeneration of the genital system - also known as "estrogenic syndrome". Male swine show signs of feminization, while female swine are more susceptible to sterility and spontaneous abortion; when offspring are produced, these are often small and weak.
- causes equine leukoencephalomalacia (brain damage and death in horses)
- pulmonary edema (inflammation of lung tissue) in swine
- cancer-causing in humans?
- associated with neural tube defects in human babies
- commonly associated with species of Fusarium found in cereal grains (particularly corn)
- Swine and other animals (especially livestock) suffer symptoms of inactivity, degeneration of the cells of the bone marrow, lymph nodes, and intestines. Leads to diarrhea, hemorrhaging (bleeding) and death.
- One form causes alimentary toxic aleukia (ATA) in humans. This results in abnormalities in blood system. ATA was widespread in rural areas in Siberia (1941-47). Toxins build-up in grain (millet) allowed to over winter in the field. Symptoms include fever, headache, diarrhea, nausea and vomiting. Hemorrhaging in various organs and parts of body worsens as disease progresses and death is not uncommon.
- Fusarium Scab in barley (and wheat) is becoming an increasing problem, especially those grains used to make malt for beer production.
- Another fungus, Stachybotrys charatum is a cellulose decomsoing hyphomycete and can contaminate hay and fodder with trichothecenes used to feed horses. Also it is know to cause hemorrhagic syndrome in the lungs of humans who breath in the spores, especially in the very young by inhibiting normal development of capillaries in the lungs. This is sometimes referred to as TOXIC BLACK MOLD, and is sometimes found on wet wood and paper surfaces in homes.
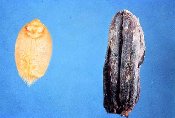
Claviceps purpurea and ergot of rye
- Claviceps purpurea and ergot of rye
- primarily on rye (sometimes wheat, barley, oats and wild grasses.
- actual damage to crop is low -fungus that causes ergot causes the seeds or grains to be replaced with dark-purple to black sclerotia.
- toxic substances produced in sclerotia including LSD (lysergic acid diethylamide) and other alkaloids.
- symptoms of eating contaminated grain referred to as Ergotism, ergot
poisoning or St. Anthony's Fire. Symptoms include, vomiting, feelings of
intense heat or cold, pain in muscles of the calf, yellow color in face,
lesions on the hand and feet, diarrhea, impairment of mental functions,
hysteria and hallucinations (possibility exists that women accused of
witchcraft and their accusers in Salem, Mass were suffering from ergot
poisoning, accounting for their bizarre behavior), convulsions, gangrene
in limbs, spontaneous abortion in pregnant women, and death. Out breaks
of ergot poisoning is not common in modern time most recent outbreak was
in Ethiopia in the late 1970's


- Some ergot alkaloids have medicinal value. Used medically to stimulate the uterus to contract to initiate child birth, an to hasten the return of the uterus to normal size after childbirth. Treatment of certain peripheral circulatory disorders, and treatment of migraine headaches. Causal agent of ergot of rye is Claviceps purpurea. Fungus overwinters as sclerotia ==> In the spring sclerotia germinate and stroma on a stalk is produced. Ascospores are shot out or extruded in a viscous fluid. Conidia are dispersed by wind and insects. Infects ovary on wild grass plant or cultivated cereal grain
- Fungus causes asexual spores (conidia) to be extruded from flower (honeydew) which is spread by insects. Developing seed replaced with sclerotium.
- For more information visit:
- http://www.botgard.ucla.edu/html/botanytextbooks/economicbotany/Claviceps/
- Linnda R. Caporael Article titled "Ergotism: The Satan Loosed in Salem?" from Science Vol. 192 (2 April 1976) at http://web.utk.edu/~kstclair/221/ergotism.html
Toxins produced by species of Aspergillus and Penicillium growing on Animal and Human Food Supplies
- Aflatoxins produced by species of Aspergillus, especially A. flavus on peanuts, maize, and other foodstuffs - CLICK HERE!
- Ochratoxins cause degenerate and necrosis of the liver and kidney in domestic animals. These may persist in the meat of animals fed contaminated grain and be transmitted through the food chain to humans.
- Tremorgenic toxins cause marked body tremors and excessive discharge of urine, followed by convulsive seizures that often end in death. Some species of Aspergillus and Penicillium growing on refrigerated foods (e.g., cheese), grains, and cereal products. Sheep, horses and cows seem to be the the domestic animals most commonly affected by tremorgenic toxins. Humans can also suffer this malady.
- Patulin is found to occur naturally in foodstuffs such as fruit or juices made with fruit partly infected with Penicillium, in naturally molded bread and bakery products, and in most commercial apple products. Patulin may constitute a serious heath risk for domesticated animals and humans. Symptoms of poisoning include, edema and bleeding in lungs and brain, damage to kidneys, paralysis of motor nerves, and cancer.
- Yellowed-rice toxins, primarily citreoviridin, citrinin, and luteoskyrin, are all produced by species of Penicillium growing in stored rice, barley, corn, and dried fish. These toxicoses are associated with various diseases, including cardiac beri-beri, nervous and circulatory disorders, and degeneration of the kidneys and liver.
Fescue Toxicosis
- Affects cattle and horses feeding on plants of the perennial grass tall fescue infected systemically with the fungus Acremonium (an endophyte).
- Horses eating tall fescue plants infected with the fungus show only reproductive disorders.
- Cattle feeding on such plants, in addition to reduced calving and lowered milk production, show reduced weight gains, elevated body temperature, and rough hair coat; feet or other body extremities may develop gangrene and drop off "fescue foot".
Bibliography on Fungal Mycotoxins in Food
-
Agrios, G. N. (1997). Plant Pathology. 4th ed.
Academic Press: San Diego.
Leslie, J. F., W. F. O. Marasas, G. S. Shephard, E. W. Sydenham, Stockenstrom, and P. G. Thiell. (1996). Duckling toxicity and the production of fumonisin and moniliformin by isolates in the A and F mating populations of Gibberella fujikuroi (Fusarium moniliforme). Appl. Environ. Microbiol. 62: 1182-1187.
Moore-Landecker, E. (1990) Fundamentals of the Fungi. 3rd. ed. Prentice Hall: Englewood Cliffs.
Rippon, J. W. (1982). Medical Mycology: The Pathogenic Fungi and The Pathogenic Actinomycetes. 2nd ed., Philadelphia.
For Additonal Information on Mycotoxins visit the following links:
- http://www.botany.hawaii.edu/faculty/wong/BOT135/lect11.htm
- http://www.nal.usda.gov/fsrio/research/fsheets/fsheet01.htm
- http://healthandenergy.com/mycotoxins.htm